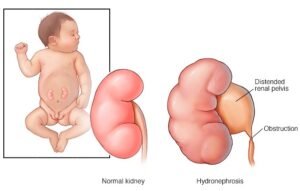
 Hydronephrosis Surgery: Hydronephrosis is a descriptive term used to indicate the presence of a distended pelvicalyceal system. It does not necessarily indicate a state of disease.
Hydronephrosis Surgery: Hydronephrosis is a descriptive term used to indicate the presence of a distended pelvicalyceal system. It does not necessarily indicate a state of disease.
The Society of Fetal Urology was the first to introduce descriptors to help assess the significance of antenatal hydronephrosis by assigning grade 1 to indicate dilatation of the pelvis alone, grade 2 to indicate that the calyces are also dilated and grade 3 to indicate that the renal parenchyma is also thinned out. In order to avoid missing any anomaly of future significance, fetal radiologists are obligated to highlight renal pelvis separation of 4mm or more in the second trimester and of 7mm or more in the third trimester as hydronephrosis. Using these criteria, an alert is recorded in 3% of babies antenatally. On postnatal followup ultrasound, the anteroposterior diameter of the renal pelvis has least interobserver variation and is used. A renal ultrasound even if normal in the newborn period should be repeated 2 to 6 weeks later due to the naturally oliguric state immediately after birth.
The urgency of referral and the need for antibiotic prophylaxis in hydronephrosis is dependent on the potential for further renal damage and infection rather than the dimension of the renal pelvis itself.
In utero transfer is advisable if there is a reduced amniotic fluid index.
Urgent /at birth referral is required if:
- The contralateral kidney is also abnormal or absent
- There is hydroureter
- The bladder wall is thickened or has an abnormality
- Bilateral hydronephrosis in a boy baby also needs urgent referral as hydroureter may not be easily picked up in antenatal or early postnatal ultrasound.
(These portend conditions with a high propensity for urinary infection and rapid deterioration of renal function and prophylactic antibiotics are indicated till evaluation rules out a low obstruction or reflux. The investigations done may include MCU, isotope renal scan and cystoscopy.) Their seriousness is now expressed as UTD 1 for the least to UTD 3 for the most serious.
Unilateral hydronephrosis with a normal opposite kidney, normal bladder and no ureteric dilatation, gives time for serial evaluation with renal ultrasound. The propensity of urine infection is so low that prophylactic antibiotics are not advised by the Indian Society of Fetal Urology regardless of the APD. Assessment is by renal ultrasound, first between 2 to 6 weeks, then at 3 to 6 month intervals. A significant pelviureteric junction is likely if the APD reaches 15mm especially if there is calyceal dilatation, more so if there is parenchymal thinning as well. The parenchymal thinning may be more severe if the renal pelvis is completely intrarenal even without the 15mm pelvis APD. An excretory isotope renal scan with diuretic renogram is done to document the degree of renal dysfunction and drainage, sometimes preceded by MCU.
Isotope scan is being in a Nuclear Medicine Lab. I am worried about radiation.
The radiation used for isotooerenal scans is the least harmful type. It is made of Beta rays counting, the type that made the hair stand up when one used to stand in front of the old types
Isn’t MCU Painful?
At KIMS, Micturating Cystourethrography is done by the paediatric urologist personally as a cinestudy under fluoroscopy. One of the parents attend the procedure. Apprehensive toddlers become playful with rectal midazolam anxiolysis.
Our surgeon said that our baby will need a hole on the side to drain urine. (Ureterostomy). Can’t it be avoided?
Neonatal valve fulguration and stenting of vesicoureteric junction obstructions obviate the need for urinary diversion in the majority. But in some with a serious degree of damage or infection, a period of drainage by Ureterostomy helps better recovery. The ureterostomy can be closed before baby starts running around.
Choice Between Open vs Keyhole Surgery for Hydronephrosis. What is best?
Open Pyeloplasty is particularly suited for babies under a year of age. The cut is only 3 to 4cm. The baby is usually smiling and ready to go home the next day. For older children, the paediatric urologist also offers laparoscopic pyeloplasty and carries the same good results. The scars are less noticeable, two chickenpox like scars, but this requires a 3 day postoperative hospital stay.

